What exactly are IUDs?
IUDs, or intrauterine devices, are small, T-shaped devices that work in your uterus to prevent pregnancy. There are 2 types—hormonal and non-hormonal, both of which can be placed by your healthcare provider during an in-office visit.
You may experience pain, bleeding or dizziness during and after placement. If your symptoms do not pass within 30 minutes after placement, your IUD may not have been placed correctly. Your healthcare provider will examine you to see if your IUD needs to be removed or replaced.
IUDs can be used by women who have and have not given birth. Once in place, an IUD provides continuous, highly effective birth control. And if your plans change, IUDs are reversible. Your healthcare provider can remove your IUD at any time and you can try to get pregnant right away. For women who use Mirena, about 8 out of 10 who want to become pregnant will become pregnant sometime in the first year after Mirena is removed.
Did You Know?
IUDs are considered one of the most effective reversible forms of birth control by the American College of Obstetricians and Gynecologists (ACOG).
Mirena is not right for everyone. Do not use Mirena if you:
are or might be pregnant; Mirena cannot be used as an emergency contraceptive
have a serious pelvic infection called pelvic inflammatory disease (PID) or have had PID in the past unless you have had a normal pregnancy after the infection went away
have an untreated genital infection now
have had a serious pelvic infection in the past 3 months after a pregnancy
can get infections easily. For example, if you:
have multiple sexual partners or your partner has multiple sexual partners
have problems with your immune system
use or abuse intravenous drugs
have or suspect you might have cancer of the uterus or cervix
have bleeding from the vagina that has not been explained
have liver disease or a liver tumor
have breast cancer or any other cancer that is sensitive to progestin (a female hormone), now or in the past
have an intrauterine device in your uterus already
have a condition of the uterus that changes the shape of the uterine cavity, such as large fibroid tumors
are allergic to levonorgestrel, silicone, polyethylene, silica, barium sulfate or iron oxide
For a full list of safety considerations about Mirena, please click here.
Addressing Some Myths with Facts about Mirena
You might have heard information about IUDs from friends, family, or even social media. Read below for the facts.
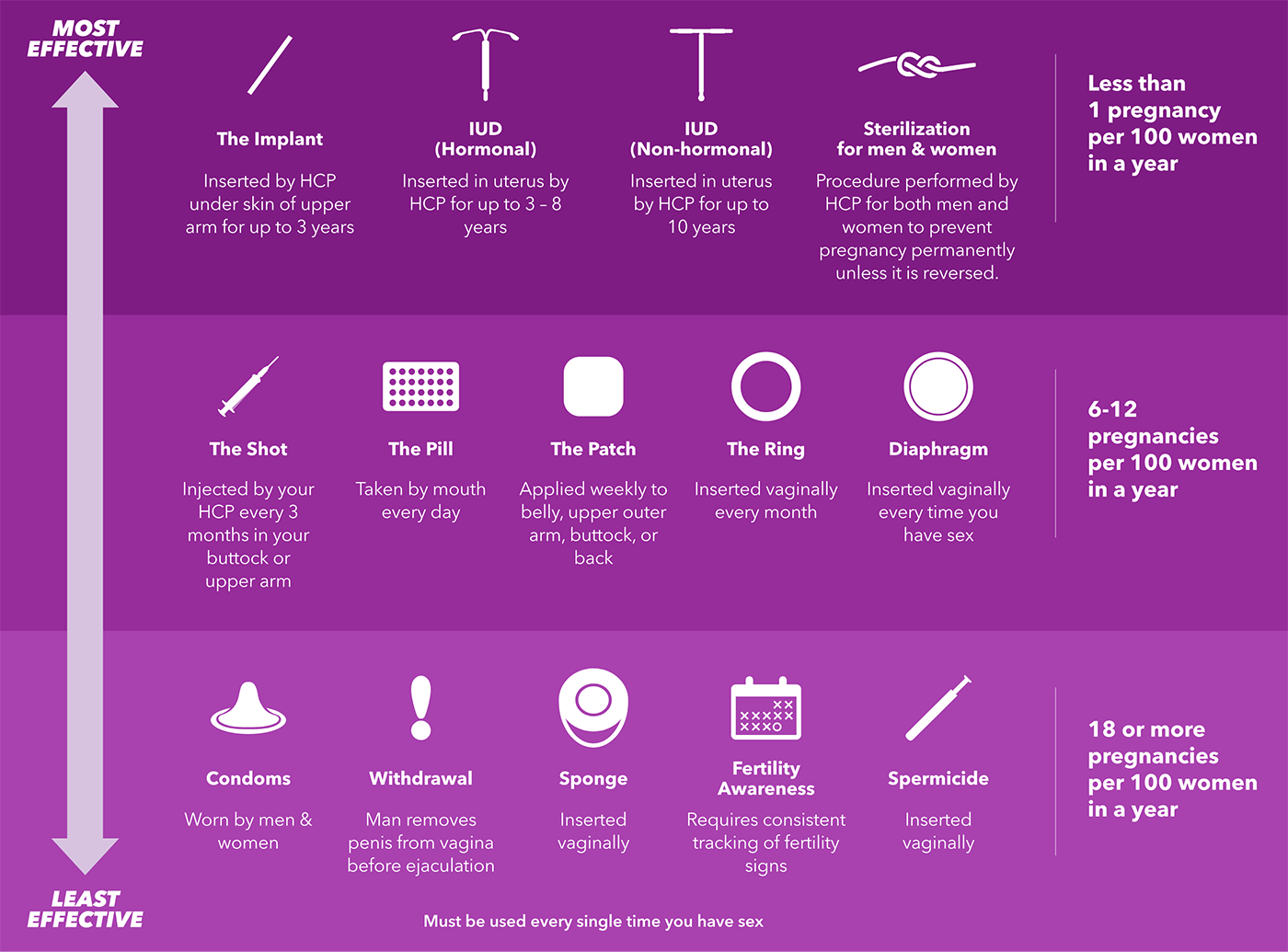
Understanding the types of birth control options
There are a lot of ways to prevent pregnancy, and it’s important to know what your options are. The chart below provides a quick overview of the various birth control options, including how each method is used and the chances of becoming pregnant. Talk to your doctor to learn more.

Is Mirena right for me?
Curious about an IUD that prevents pregnancy for up to 8 years and treats heavy periods for up to 5 years in women who choose an IUD for birth control?
INDICATIONS FOR MIRENA
Mirena® (levonorgestrel-releasing intrauterine system) is a hormone-releasing IUD that prevents pregnancy for up to 8 years. Mirena also treats heavy periods for up to 5 years in women who choose intrauterine contraception.
IMPORTANT SAFETY INFORMATION
- If you have a pelvic or genital infection, get infections easily, or have certain cancers, don't use Mirena. Less than 1% of users get a serious pelvic infection called pelvic inflammatory disease (PID).
- If you have persistent pelvic or stomach pain, or excessive bleeding after placement, tell your healthcare provider (HCP). If Mirena comes out, call your HCP and avoid intercourse or use non-hormonal back-up birth control (such as condoms or spermicide). Mirena may go into or through the wall of the uterus and cause other problems.
-
Pregnancy while using Mirena is uncommon but can be life threatening and may result in loss of pregnancy or fertility.
- Ovarian cysts may occur but usually disappear.
- Bleeding and spotting may increase in the first 3 to 6 months and remain irregular. Periods over time usually become shorter, lighter, or may stop.
Mirena does not protect against HIV or STIs.
Only you and your HCP can decide if Mirena is right for you. Mirena is available by prescription only.
For important risk and use information about Mirena, please see Full Prescribing Information.